![]()
 |
|
Preventing a Migraine Headache
Migraine prophylaxis or migraine prevention refers to trying to prevention migraines from occuring in the first place. For some, this means preventing any symptom of migraine from occuring. For others, it includes intervention that begins at first symptoms (think food craving, yawning, neck pain, aura, or other minimal head pain). There are many layers to the therapy. Some things that the patient does for themselves, some things that involves the physician raising the threshold to get any migraine symptom in the first place, and then finally, a strategy to attack the migraine at its earliest stages before it can cause any disability.
It is critical that the patient has a physician who listens to them and takes a history as to the number of headache free days and not just the "migraine days" or severe headache days. Dr. Loftus thinks of migraine treatment as a "team sport" and it is most critical in patients with frequent migraine requiring a prevention. See what Dr. Loftus' patients say about his practice here.
Rebound headache is a type of daily headache which occurs from the overuse of migraine medications. Basically, the medication itself becomes the cause of the next trigger. It is fortunately very infrequent and easy to treat if the rebounding agent is a triptan, caffeine, or an NSAID. It is much more difficult to treat when the offending agent is a narcotic or contains butalbital. The use of prophylaxis in patients having more than 2 headaches per week should be universal even if the headaches are not particularly disabled, particularly in those younger than 40 since headaches tend to get worse as one approaches the early 40s. Many patients with 1 - 2 headaches per week will need prevention unless the patient is disability free. In some patients having even one or two disabling headaches each month is enough to justify migraine prevention if they are severe enough to put the patient to bed.
The first step of prevention is trying to eliminate the common triggers. Ask yourself the following questions. Do I get regular sleep? Do I skip meals? If I travel across time zones, do I try and prepare my body for this before I leave? Do I have a strategy when I get there? Are there specific foods that I eat that I know trigger a headache? The most common food triggers are caffiene and possibly chocolate. While many triggers are not possible to avoid, such as weather changes and outside stressors, minimizing those that you can to something about is commonly very helpful when one is beginning to try and better manage their migraine disability.
Once the lifestyle preventative measures have been considered, the next most important step is to make sure the patient is not potentially having rebound headaches. Any medication that is being taken twice or more weekly could potentially be causing rebound headaches. Usually, rebound headache are causied by medications taken on a near daily basis. Rebound headaches from triptans and NSAIDs have never been shown to interfere with migraine prevention. Rebound headaches from opioids and butalbital do interefere with attempts at prevention. Many times, a low rebounding but less convenient medication - such as the injectable NSAID ketorolac or injectable dihydroergotamine is used to substitute for the potentially offending agent. Many times a multi-layered approach at prevention is tried first before proceeding to a more formal medication discontinuation trial when the risk of rebound is low (triptans, NSAIDs) or the acute pain is high and the patient feels they have to have it.
How Can I Help My Doctor Help Me
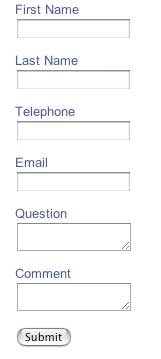
You need to gather real time information on your headaches. Your physician needs the number of headaches, medication usage, and disability. It is also helpful to have your headaches properly classified. Dr. Loftus designed the iPhone and iPod touch app iHeadache to do all of this for you. The value of iHeadache is that it will produce reports that you and your physician will be able to use to properly diagnose your headache, determine if prevention is warranted, and to determine over time if therapy is working. An Android version and web based version is currently under developement.
There are now many types of prevention available. If cost is the primary consideration, then there is a number of oral therapies available. There are quite cheap with even cash prices without insurance running less than $20 per month. When oral therapies are not desired, there are a number of migraine procedures that can be done. Some of there are $100 per month. Finally, we have the injectable Botox, Monoclonal Antibodies against CGRP (MAAC - Ajovy, Emgality) or its receptor (MAACR - Aimovig). These medications are $500-600 per month. At Bellaire Neurology, the ultimate decision is made between the patient and Dr. Loftus depending on cost, comorbid diseases (other disease present such as depression, anxiety, fibromyalgia, asthma, and epilepsy), patient weight, potential to get pregnany, and potential of known risks and unknown risks of the various therapies.