 Pain that occurs secondary to pressure within the nasal sinuses typically is located over the involved sinus area. This pain is constant, even, and not throbbing. It is also not associated with nausea, light, or noise sensitivity like migraine headache. Accompanied by fever and a purulent discharge (discolored yellow or green), the pain is usually caused by acute sinusitis. The treatment of sinusitis is somewhat controversial because the majority of the causes are not bacterial and the overuse of antibiotics is an increasing concern. When it is bacterial, antibiotic treatment as well as surgical drainage of the infected sinus may be required.
Pain that occurs secondary to pressure within the nasal sinuses typically is located over the involved sinus area. This pain is constant, even, and not throbbing. It is also not associated with nausea, light, or noise sensitivity like migraine headache. Accompanied by fever and a purulent discharge (discolored yellow or green), the pain is usually caused by acute sinusitis. The treatment of sinusitis is somewhat controversial because the majority of the causes are not bacterial and the overuse of antibiotics is an increasing concern. When it is bacterial, antibiotic treatment as well as surgical drainage of the infected sinus may be required.
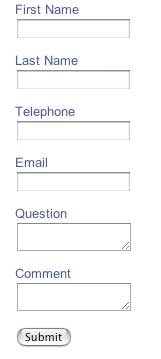
If you have recurrent sinus headaches, then Dr. Loftus strongly recommends tracking your symptoms in real time to determine your headache type. He has designed the iPhone or iPod touch app iHeadache to do this. iHeadache will keep track of your symptoms, medications, and disability and the "artificial intelligence" of the program will help classify your headaches.
Dr. Cady published a study in the Journal of Neurology {Cady R, Schreiber C, Neurology 2002 58:Suppl 6,S10-15} on a group of patients who came to him with self-diagnosed or physician-diagnosed sinus headaches. They were all adults and also had at least a one-year history of recurrent headaches. The patients in this study were having on average at least one headache per month. They were excluded if they had fever, a discolored nasal discharge, or radiographic (X-ray or CT) evidence of sinus infection. They were also excluded if they had ever been diagnosed or treated for migraine headache. These patients were also required to have at least one of the following symptoms:
- Moderate to severe pain
- Pain increasing with activity
- Unilateral pain
- Nausea/vomiting
- Sensitivity to light or noise during the headache
- Throbbing or pulsating pain
Out of the group, 46 out of 47 patients met the International Headache Society (I.H.S.) Classification {Cephalgia 2004;24 (Suppl 1)} for Migraine or Probable Migraine headaches. They responded to Imitrex® in a manner that prior migraine studies would have predicted. The patients and their prior physicians probably felt they had sinus headaches because 87% reported nasal stuffiness and/or nasal drainage with their headaches. Nearly half (45%) felt that weather changes were a trigger for their headaches as well.
Another study known as the SUMMIT study analyzed over 3000 patients who presented to their primary care physician (98%) with self-diagnosed or previously physician diagnosed recurrent sinus headaches. Of these, 88% had either IHS migraine or probable migraine. Exactly 8 had sinus disease. This data has only been presented in a poster format at the June 2002 American Headache Society meeting. Patients who had the HIS definition of migraine were then treated with sumatriptan and the results were that 2/3rds of patients were satisfied with their headache therapy after treatment with sumatriptan. Prior to treatment with sumatriptan, 2/3rds of patients were dissatisfied with their current treatment.
Another study of headache patients in the United States showed that only 52% of Americans with migraine headaches knew they had migraine. Of those that did not know they had migraine headache, the largest group had been misdiagnosed with sinus headaches. One reason for the large group of misdiagnosed patients is the disagreement between the ENT medical society's definition of rhinosinusitis and the International Headache Society Classification of Migraine and Probable Migraine Headaches. In fact, the patients in Dr. Cady's study probably fulfilled the ENT criteria of rhinosinusitis. The World Health Organization, as well as societies representing Internal Medicine, Family Practice Medicine, and Emergency Medicine, among others has accepted the I.H.S. system.
If you experience both migraines and sinus headaches then please discuss using your acute migraine medicine for both your sinus and migraine headaches with your physician. Also ask your physician if he or she feels you have two separate diseases, i.e. recurrent sinus headaches and migraine. If your physician feels you do have two seperate diseases then consider getting a second opinion from a neurologist.
If you only have recurrent sinus headaches, then please review either the entire migraine section or the section on the diagnosis of migraine and probable migraine headaches to see if you fulfill these criteria. If you do fit the criteria then please see your doctor because there are very good medications available for both acute treatment and prevention of these headaches.